All You Need to Know About Stroke Recovery
This ultimate guide to stroke recovery will provide important information about healing from a stroke. It includes sections on what types of strokes there are, symptoms that indicate one has occurred, and steps for rehabilitation after experiencing them to maximize functional levels as quickly as possible!
The World Health Organization estimates that over 4 million people suffer from a stroke each year, but there is hope. Over 10% of those who experience a brain attack will fully recover some abilities. In comparison, 25 percent achieve slight impairments and 40% moderate to severe losses in function or appearance due to their condition at initial presentation without any permanent effects on personality traits whatsoever!
It’s always challenging to hear that somebody you care about has been affected by a stroke. It impacts life and often changes it forever – but the good news is there are ways to get back some abilities. Studies show that 10% will fully recover while 25 percent will maintain most aspects of daily living without severe restrictions; 40+ percent will have moderate to severe impairment.
The goal of stroke recovery is not just to get back on your feet but also to continue that momentum. For this process to be successful and sustainable, you will have to commit through patience, perseverance, and hard work; these three factors play integral roles in achieving success!
This book will detail the equipment you will need and what to expect. However, the primary action you must take is assembling the right team to assist in your recovery efforts. The proper medical, rehab support, domestic help, and emotional support are essential in helping you to maximize your capabilities.
The physical rehabilitation of stroke survivors is critical to their daily life. They have many concerns, including mobility, speech, medication management and finances. All things that need attention to make this journey as manageable as possible! This guide will help you understand how physiotherapy can be an essential part of your overall recovery process following a traumatic brain injury, so don’t hesitate to get started on what comes next by reading more about it here.
Recovery from a stroke is difficult. It requires hard work and dedication. However, the rewards to yourself and the people you love will be worth all the hard work. If you are a loved one of someone who has suffered a stroke, be strong and help them along. The journey will not be easy, but it might be life-changing.
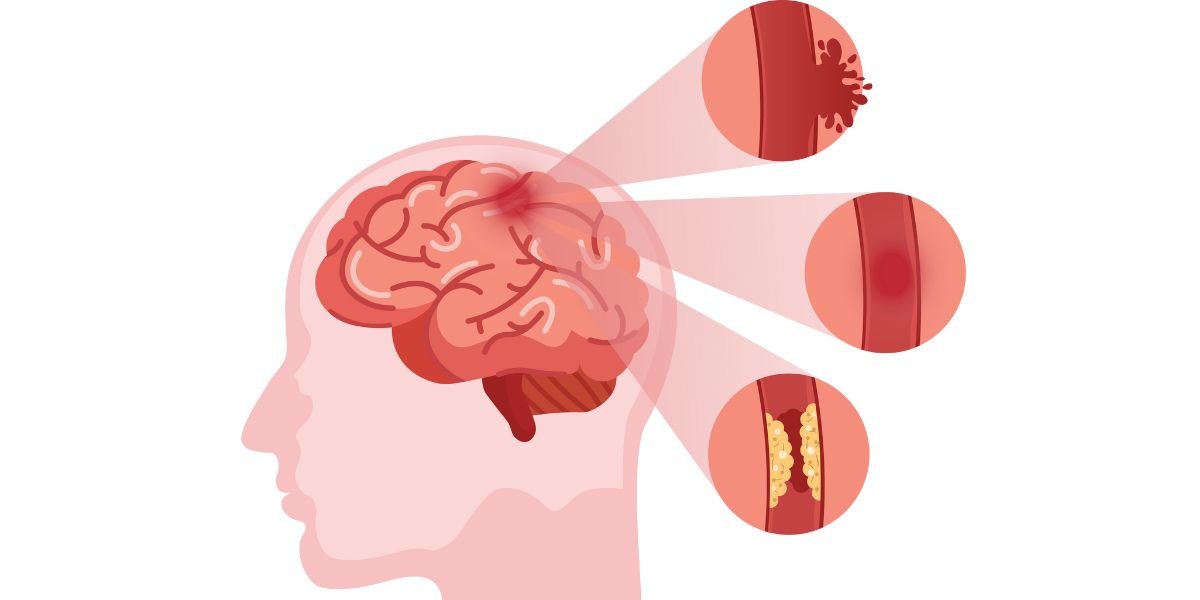
What is a Stroke?
A stroke is a brain injury. Strokes can be called a brain attack. They occur when blood supply to sections of the brain is interrupted or reduced. Our brain is the nerve center that controls our thoughts, movements, and our body’s vital organs. The severity of the damage will depend on the type of injury and the location. More minor strokes might have little to no symptoms. Larger strokes can be life-changing. Approximately 10% of people will die from a stroke.
The brain is the most important organ in our body. It controls everything from heart rate to digestive system functions and even postures! A stroke can happen when there’s not enough blood flow for an area of tissue called the “brain.”
Brain tissue damage caused by a stroke interferes with nerve cells slowing or stopping their communication ability. Brain cell health is vital for our bodies to function optimally.
The body’s cells cannot get enough nutrients with this lack-of oxygen. The result is damage affecting other abilities such as speech or movement, becoming impaired after time had passed from when the stroke occurred.
After a stroke, the first step of rehabilitation should be rewiring your brain. The process known as neuroplasticity helps in this endeavour by encouraging new pathways that were not there before and emphasizing the importance of beginning early on with physical therapy after experiencing such an accident or illness so you can get back on track quickly!
Our bodies are exceptional engineering works, and the ability to regenerate new neuro-pathways is a prime example. However, it is only through forcing our brains to rewire themselves that this magic can happen. Rehab starts in the brain and not the body. If you have a problem moving your arm or leg, you might assume the problem lies in the muscle. However, the problem likely resides in the damaged brain. Through the repetitive movement of these muscles, your brain can learn to control the movement of the affected body part. Physiotherapists are experts in helping the brain speak to the body.
What Are The 3 Types of Strokes?
No two strokes are exactly alike, and as a result, no two outcomes are similar as well. The location, the severity and permanence of the blockage all contribute to the effects of a stroke. There are three main types of strokes, and each has a different cause and effect.
Approximately 85% of all strokes are ischemic. Ischemic strokes result from a blood clot blocking blood flow to the brain. Arteriosclerosis often causes blood clots that originate elsewhere in the body. This blood clot breaks off and travels to the brain, blocking the blood supply. Lack of oxygen to the affected area of the brain will cause the cells to die. Once cells begin to die, the brain will lose control of the affected area. Regenerating new pathways and rewiring the brain is possible. Successful recovery depends on the severity of the blockage, the location, and your rehabilitation quality.
Approximately 15% of all strokes are hemorrhagic strokes. Hemorrhagic strokes are more severe than ischemic strokes. Hemorrhagic strokes result from burst blood vessels in the brain, or if a weakened blood vessel begins to leak, unfortunately, around 40% of all people who have a hemorrhagic stroke die. Hemorrhagic strokes are usually a result of high blood pressure or the use of blood thinners. The prognosis of recovery from hemorrhagic strokes is less promising than ischemic strokes. Approximately 12% of people can fully recover from such a stroke.
The third type of stroke is a transient ischemic attack or TIAs. Doctors refer to TIAs as mini-strokes. TIAs cause temporary blockage of a blood vessel and usually result in no lasting damage. Transient ischemic attacks are a warning sign that a potentially more significant stroke might occur. It is essential to take these small strokes seriously as a change in lifestyle could avoid a major stroke in the future.
What Causes a Stroke?
Ischemic strokes are the most common type of stroke, separated into two categories, thrombotic and embolic strokes. Both of these types of strokes have different origins. Arteries within the brain that are blocked are thrombotic strokes. They further divide into large-vessel thrombosis or small-vessel thrombosis. Large-vessel thrombosis is when there is a blockage to a major artery that supplies blood to the brain, a small-vessel thrombosis is a blockage of smaller arteries.
Large-vessel thrombosis is the most common type of stroke. A thrombotic stroke of a more significant artery will also affect the smaller arteries that feed off the main artery.
Atherosclerosis is the primary cause of blood clots. Atherosclerosis is a disease with a buildup of plaque in the arteries. Plack buildup on the artery wall, blood flow can slow or stop, resulting in a blockage. There are a few reasons for plaque to form on the artery wall, including high blood pressure, high levels of LDL cholesterol, and low HDL cholesterol levels. Diet, smoking and a sedentary lifestyle are also considered risk factors for atherosclerosis.
Embolic strokes occur when there is a blockage somewhere other than the brain. A portion of the clot breaks away and travels through the body to the brain. Often this blockage originates in the arteries near the heart. High blood pressure is the leading cause of embolic strokes.
Hemorrhagic strokes are a weakening or a bursting of an artery in the brain itself. These strokes are severe and have a higher rate of death. The leading cause of hemorrhagic strokes is high blood pressure.
Proper diagnosis is critically important for your treatment and rehabilitation. Treatment of a hemorrhagic stroke is different from ischemic stroke. It is dangerous to treat an ischemic stroke survivor like a hemorrhagic stroke survivor and vice versa.
Make sure to get a proper diagnosis of your stroke and ask your medical team for the precise details of the diagnosis. Physiotherapists can then work from that diagnosis to accurately layout an exercise program that is ideally suited to your particular stroke.
High Blood Pressure is The Leading Cause of Strokes
For most people, high blood pressure is an easy problem to manage. However, if left unchecked, it can lead down a dark path ending in stroke for those who don’t.
Strokes are sudden and violent events that occur when brain cells die due to a loss of oxygen. The most common cause of this lack of oxygen is blood clots that block the arteries supplying the brain with blood. Many of these blocks occur in arteries leading to the brain because they are smaller than those elsewhere in the body, so blood clots more easily build up there. High blood pressure deforms and damages these and other arteries and weakens their walls over time. All of this leads to an increased risk for stroke.
So long as the patient takes measures to control high blood pressure—such as exercising, keeping a healthy weight, avoiding smoking, and limiting alcohol consumption — they should not have to worry about stroke.
If you are someone you know may be at risk for stroke, talk to your doctor about how to keep your blood pressure down and avoid this serious health concern.
What Effects do Strokes Create?
We know that there are a few different kinds of strokes and that each has its unique origins and corresponding damage to the brain. No two strokes are the same regarding the brain damage done and the lasting effects. However, strokes do have some similarities.
The critical determining factor of the effects of a stroke will depend on the exact location in the brain and the duration of time the artery was blocked.
How our brains control movement is quite fascinating. The right side of the brain affects what you do on your left, and vice versa for both language processing (like speech) and motor skills; one may suffer paralysis while another doesn’t lose any function at all!
A brain attack has many other detrimental effects on how we behave; one result being quicker thinking processes coupled with more significant amounts of spent time considering possibilities
The right side of the brain controls personality traits like quickness and inquisitiveness. If this area is affected by a stroke, people may show more signs that they’re in a hurry or trying hard to think through something quickly than those on the left side who has slowed down mentally due to their injury
The left side of the brain is responsible for our ability to think and respond. If you have had a stroke in this area, it can affect your mental skills, such as communicating with people or reacting quickly in an emergency.
Strokes in the central brain stem can cause paralysis throughout your body. If you have a stroke at another location, it will only affect specific muscles and parts of movement like slowness or difficulty speaking clearly.
A stroke situated to the back part of the brain may damage vision. The damage caused by a stroke can be permanent, and vision loss is the most common result. The brain controls everything in your body, so many things go wrong with both movement & balance and mood swings, among others, when it’s injured or damaged.
It is important to remember that our bodies are capable of retraining pathways after a stroke. However, it is essential to note that you can alter even severe paralysis. Although not all effects of a stroke may be reversible, changes in speech and movement are possible.
14 Most Common Symptoms Of A Stroke
A stroke is a disease caused by interrupting the blood flow to the brain. There are two types of strokes: ischemic and hemorrhagic. Symptoms of a stroke vary depending on whether an individual has had an ischemic or hemorrhagic stroke.
The most common stroke symptoms for both types are:
Sudden confusion
Trouble speaking
Difficulty understanding speech
Difficulty seeing (partial or total blindness)
Balance issues
Weakness in arms or legs
Numbness in the face
Severe headache
Slurred speech
Difficulty swallowing
Sudden dizziness
Altered mood, either sudden depression or euphoria
Irritability
Drowsiness
An ischemic stroke occurs when a blocked artery starves the brain of oxygen-rich blood. Ischemic strokes are more common than hemorrhagic strokes, but both can cause serious complications. When a clot breaks loose and blocks blood flow to part of the brain, it results in cell death (infarct). A hemorrhagic stroke occurs when a blood vessel in the brain ruptures and leaks, causing pressure to build up.
In either case, the lack of oxygen from reduced or interrupted blood flow can damage nerve cells in the brain and cause permanent disability.
Symptoms of a stroke vary widely. Factors that affect which symptoms appear are:
The amount of blood supply to the brain that is blocked
The location of the blood clot
If there are hemorrhages in the brain
If you or a loved one experiences any of these symptoms, you must act swiftly to summon emergency services.
Stroke Facts
Strokes are prevalent in Canada and all over the world. In Canada, there are approximately 62,000 strokes annually. Worldwide, strokes affect over 15 million people each year. One in six men and one in five women will suffer a stroke in their lifetime.
In Canada, someone has a stroke every 10 minutes. Approximately 80% of stroke victims survive.
Strokes are devastating events that can happen at any age, with the majority occurring before 60 years old. However, it is essential to note that there have been cases documented where people in their twenties experienced a stroke due to pre-existing conditions like hypertension or heart disease, making them more susceptible.
For every 6300 babies, one is born with a stroke. In Canada, there are currently over 10,000 people under the age of 18 living with the effects of a stroke. The occurrence of strokes in infants and youth points to a pre-existing condition.
Men are more predisposed to strokes than women until they reach their early to mid-eighties. After 85, women are more likely to have a stroke.
There is a sharp increase in stroke rates as baby boomers begin their retirement years. As this happens, death from strokes will decrease with new medications and treatments available to the general public now more than ever before!
There’s going to be an even greater demand for medical assistance among those who survive these life-threatening conditions – which will put pressure on our healthcare system overall and require more vital collaboration between all professionals involved.
It’s never been clearer: Strokes Are Dangerous.
Your Hospital Stay After a Stroke
Most stroke survivors will arrive at the hospital via the emergency department. These first few hours are vitally important to your recovery in the days, weeks, and months afterward. Your time upon arrival will no doubt be terrifying and confusing.
The primary goal is to keep you alive. Doctors and nurses will ensure you are receiving adequate blood flow. They will monitor both your breathing and blood pressure. The medical team will work to stabilize you before they begin to diagnose the nature of your stroke and order a CT scan. The scan will show both the location of the stroke and the type of stroke. This information is critical in your treatment.
If you have suffered an ischemic stroke and a clot caused the stroke, the attending physicians will consult on whether or not to administer a tPA drug. Tissue Plasminogen Activator is a clot-busting drug. Ideally, doctors will administer this drug within a few hours of a stroke. Taking early tPA can reduce the damage and even reverse some of the long-term effects of strokes.
Endovascular Thrombectomy is a surgery that can help to restore blood flow and relieve pain. Surgeons insert thin tubes into your veins, which they follow until they meet an obstruction such as clots or other causes for blockages in arteries; then, reopening occurs once the surgeon removes all of the blockages.
Early Intervention Is Critical
After a stroke, a critical time for rehabilitation is the first few days, weeks, and sometimes even months. Losing functional use of your arm or leg can be a devastating blow to your independence which means that early intervention will have lasting repercussions on future quality of life. Immediately receiving appropriate care ensures patients aren’t held back by lacklustre recovery efforts later down the line.
Many people don’t realize how life-threatening a stroke can be. The first few hours after a stroke is critical for either clot-busting drugs or surgery to remove the blockage in your blood vessels that caused it, but if you’re not there when they need help – many will never make it out alive!
Most Canadians are unable to recognize the signs of a stroke. The symptoms of a stroke include; trouble speaking and slurring of words, sudden weakness in the face, arms, and legs, vision problems, sudden severe headache, and dizziness. Someone who has suffered a stroke may show one or more of these symptoms.
Hospital stays for blockages vary depending on the severity of damage and location. The length in hospital can be anywhere from one day up to several months, but it’s usually about three weeks or less at most!
The pathway through the hospital may involve the emergency department, acute care, complex continuing care, and inpatient rehab. However, your rehab work will continue during your entire stay in the hospital. This period is significant as you begin to repair the damaged circuitry from your brain to your working muscles.
Your first session with a physiotherapist will involve an initial assessment. This examination allows the therapist to understand your physical abilities, identify any safety concerns and create personalized treatment plans tailored just for you! The session might include:
A mobility test to determine how the stroke has affected your movement patterns.
A swallowing test to determine if the stroke has impacted your swallowing ability.
A balance test to see if the stroke affected your balance.
A communication test to see if the stroke affected your speech.
A cognitive test to determine if the stroke has affected your critical thinking.
A skin test to determine if there are concerns regarding pressure areas that could cause ulcers or sores.
A test for strength and endurance.
The initial assessment will lead to a comprehensive rehabilitation plan.
The inpatient physiotherapist will develop this plan in co-operation with the attending physicians and the nursing staff. This assessment may occur in the acute care unit, complex continuing care unit, or the inpatient rehab unit.
Your rehabilitation team may involve many different healthcare professionals depending on your needs. The list may include doctors, nurses, physiotherapists, occupational therapists, speech pathologists, dieticians, psychologists, pharmacists, social workers, and rehab assistants. Each health care professional brings a different skill set, and the team must work in unison with the patient to deliver the best possible outcome.
You will begin the critical initial stages of your exercise routine during your stay. Some days will be more challenging than others, and improvements might seem slow or non-existent. However, don’t get disheartened and focus on the progress you see and feel.
Stroke recovery can be long and arduous, but you owe it to yourself and your loved ones to stay resolute. Stroke recovery is all about repetition, repetition, and never giving up. You are a crucial part of your team. Your motivation is the single most important determining factor of success in your stroke recovery.
Preparing Your Home After a Stroke
What should you prepare for when a loved one has had a stroke? The most important thing is to make sure the home environment will be able-bodied and safe.
No two strokes are the same, and no two outcomes are similar; every stroke survivor will have limitations and specific needs. However, it is vital to have your home modified to your situation before being discharged from the hospital.
Safety should be the primary objective. Comfort and convenience are other keys to keep in mind. Modifications to the home should try to match the abilities of the stroke survivor to that of the home environment.
An occupational therapist can assist you in assessing your physical abilities and recommending changes to your home. Occupational therapists are experts in identifying and altering roadblocks that hinder people from doing important things in their lives.
Occupational therapists understand your current state of health, your rehabilitation and environmental needs, and find solutions to assist you in moving forward. Your medical team can help you in obtaining assistance from an occupational therapist.
Home renovations can be costly and time-consuming. They can involve entire floor planning and expensive equipment or simple modifications and minor adaptations. Safety and ease of use must be the main focus.
Here is a checklist of considerations for preparing your home on the following page:
Kitchen
Have lightweight containers available for storage and reheating.
Place a microwave on the counter within easy reach.
Cooktops with a smooth surface reduce the need to lift pans onto a burner.
Attempt to keep most items between 30 and 54 inches from the floor.
Turn the hot water temperature down to avoid burns.
Wall ovens are preferable if installed at the appropriate height.
Arrange food in the refrigerator so that it is accessible.
Rearrange the shelving so that the shelves work for you.
Make sure that the freezer is reachable.
Employ a small cart or trolley to transport items.
Arrange a chair or stool in the kitchen to sit while preparing meals.
Prominently place a calendar to track all of your appointments.
Write down significant numbers and make this visible.
Rearrange the pantry so that most items are within this height.
Utilize lazy susans that allow for more storage in the cupboard.
Bathroom
Remove any loose throw mats.
Install grab bars along the wall and the shower area.
Have a transfer bench if you have a tub/shower.
Non-slip floor mat outside the shower.
Non-slip floor mat inside the shower or tub area.
Install a hand-held shower head for more accessible bathing.
Install a raised toilet seat or commode.
Place all toiletries within easy reach, above 30 inches, and below 54 inches.
Bedroom
If stairs are in the home, consider moving a bed to the main floor.
Make sure there is a clear path to the washroom.
Remove all items that could cause a fall.
Take away all throw rugs and secure others with double-sided tape.
Make your clothes more accessible by lowering the bar in the closet.
Rearrange the dresser to place the most commonly used items within reach.
Make sure your wardrobe contains clothes that are easy to put on and take off.
Consider a commode to avoid a nightly trip to the washroom.
Overall
Review the entire home with safety in mind.
Tape down or remove all rugs.
Make sure rooms, halls, and walkways are well lit.
Remove any furniture that blocks pathways.
Have remote controls for all of the electronics easily accessible.
Provide a chair by the door to make putting shoes on more accessible.
Have a portable phone or cell phone.
Program emergency numbers and close family and friends into the phone.
Coming Home After a Stroke
Having a proper discharge plan before leaving the hospital will ensure your safety and improve your recovery. Your doctor will discharge you to a rehabilitation unit, long-term care facility, or back to your home. Before discharge, it is essential to have your in-home medical team already assembled.
Your social network of family and friends will be crucial in the time after arriving home. They will observe any noticeable changes in your physical and emotional states. It might be stressful after leaving the hospital, and it is essential that proper planning precedes the move.
When you survive a stroke, it is vital to make sure your recovery goes according to the plan and that any lifestyle changes are made not to increase the chances of having another. Strokes can happen again and often without warning signs beforehand – which means prevention isn’t enough; education will help too!
Be mindful of possible changes in your emotional state. After a stroke, it is pretty common to experience sporadic emotional outbursts. Many stroke sufferers experience negative emotions, and if this occurs, you should consult with your physician. Unfortunately, emotional complications can be a side effect of strokes, and most stroke survivors are not made aware of this.
You may be allowed to visit your home before being formally discharged. A visit home will allow you and your family to assess precisely the necessary steps needed before full discharge.
Equipment You Will Need
The equipment you will need in your home upon discharge depends on the severity of the stroke and the limitations caused by the stroke. Likely, all or some of your mobility, strength, vision, cognition, and movement have been affected. Devices and equipment can help keep you safe, assist in performing daily tasks and provide a degree of convenience.
Your mobility should be your primary concern. Frequently, following a stroke, getting around the house may become difficult or almost impossible. Depending on how much assistance you require, a mobility aid can help you move about your home. A stroke survivor may graduate from one mobility aid to another as their recovery progresses. For those who have difficulty walking or are at risk of falling, a wheelchair might be advisable. Ensure that the chair fits through doorways and turns in halls and small rooms. If you have suffered weakness in your arms, at times, an electric wheelchair might be a better option.
Walker or Rollator?
A walker or rollator is ideal if you need assistance moving around your home. A walker is not a rollator, nor is a rollator a walker. Walkers are support devices that have four solid legs and provide more support than rollators. However, walkers require a strong upper body to move them each step of the way. Rollators have wheels and offer less stability than walkers but are easier to push along. Rollators come with a handy basket to carry items from one room to another.
Picking The Right Cane
A walking cane is likely suitable for walking but could use additional support. Canes come either with a single tip or a 4 point tipped end. Make sure your cane is fitted correctly and used correctly. If able, you might consider using the cane on your affected side to stimulate weight bearing on your weaker extremity.
Whatever device you choose to use, proper fitting and correct use are essential for your safety and recovery. Physiotherapists will ensure which aid is appropriate and correctly fit your body size. Practice with the physiotherapist to use the device safely and practically.
Additional items to consider:
Leg lifter to move a weakened leg on and off a bed or couch
Fall prevention socks
Long handled shoehorn
Sock aids
Adaptive eating utensils
Bibs and clothing protectors
Tables that can go over a couch, chair, and bed
Handwriting aids
Programmed cell phone
Medical alert
Medication reminders
Wheelchair and rollator accessories
A reacher or grabber for the kitchen, bathroom, and or the bedroom
Many medical aids can aid the transition from the hospital to your home. Thoroughly analyze your needs and purchase those items that will go a long way to helping yourself to be as independent as possible. It is essential to buy these items before discharge. Once the stroke survivor has settled in at home, you can make the necessary adjustments.
Chances of Recovery
If you have suffered a stroke and that stroke has robbed you of some abilities, your first question might be, ‘Will I ever recover?’. Your doctor might give you guidelines about the capabilities you may regain or your recovery timeline. However, the bottom line is that no one knows as there are too many variables associated with your recovery.
There are three prime considerations to consider when assessing the chances of a positive outcome. The severity of the stroke, the quality of your rehabilitation, and the degree to which you are personally motivated.
We have always known that recovery is possible, but the goalposts keep shifting on what we can achieve. For decades, doctors believed stroke survivors only had a maximum of six months to make progress with their disabilities before it would become impossible for them to improve further; however, recent research suggests otherwise!
This information has given hope not only to those who suffer from these terrible accidents–although they deserve every chance at success!–but also to people like you.
Stroke survivors can regain much of their prior abilities within three months after a stroke if they are in the moderate category. Approximately 40% will take longer than this for complete recovery, but there is hope! Severely impacted people may need up to one year or more before regaining all functions. However, it’s possible with hard work and dedication from both family members, medical professionals and stroke victims to get back on track towards independence once more.
The quality of your care matters greatly. Working with a rehab team, whether in a clinic setting or your own home, is crucial to obtaining the best possible outcome. Physiotherapists can assist survivors with expert knowledge and guidance that accelerate the pace of recovery.
Rehabilitation is a necessary part of the recovery process. Working with an experienced team, whether in a clinic or at home, will give you a tremendous advantage in the weeks and months ahead.
The most significant variable is your attitude and your determination. It begins with the outcome your doctor has given you. The diagnosis is merely a guideline, and it doesn’t mean you can’t exceed their predictions. Take whatever your doctor says with a grain of salt. Surround yourself with positive people and positive energy. The road to recovery is challenging and arduous, but you owe it to yourself and your loved ones to stick to the plan.
Repetition is critical, and while this may become monotonous, it is essential to reconnect those neuro-pathways between your brain and your body. Your attitude and your effort are the single most significant determining factors in the success of your rehabilitation.
Role of a Physiotherapist
Assembling the right support team during your rehabilitation is vital in maximizing a positive outcome. A stroke support team may consist of medical professionals and family and friends.
Professionals can include physiotherapists, speech therapists, language therapists, doctors, and nurses. The team must work as one with a singular goal, achieving the best possible outcome for you. Ensure that the professionals who assist you have experience with stroke rehabilitation and maintain a positive attitude.
A physiotherapist will be integral in your rehabilitation. Once damage to the brain has occurred, and cells die, they do not regenerate. However, physiotherapists are experts in helping the brain create new pathways to work together for your brain and body.
Following a stroke, it is vital to regain balance and coordination by restoring past movement patterns. A physiotherapist’s role is to return as much normal function as possible and allow you to return to the activities that you enjoy.
A physiotherapist will begin with a thorough assessment to gauge where your limitations are at present. The therapist will then develop a treatment plan and discuss your goals. Physiotherapists will show you proper movement patterns and suggest alternative methods to perform everyday tasks.
A physiotherapist will guide family, friends, and support staff to assist and take part in daily exercises. Physiotherapists will teach you how to use mobility aids and help to advise on safety measures.
Ensure your chosen physiotherapist has expertise in stroke recovery and that they share your goals. Physiotherapists are vitally important in your long-term success.
Neuroplasticity
Neuroplasticity is the ability of your brain to change itself. Our brains do indeed have a tremendous amount of neuro rewiring capabilities and can develop new connections after suffering a stroke.
Twenty or thirty years ago, the belief was neurological pathways were rigid and that damage was irreversible. However, thanks to discoveries in neuroscience, this has proven to be false. Our brains do indeed have the ability to change and develop new connections. Neuroplasticity means brain reorganization.
Let’s examine how we walk. We have been walking since we were very young. An adult does not need to imagine putting one foot in front of the other or lifting our thigh and bending our knee. We do this unconsciously, and there is very little need to think about this process. However, as a young child, you did need to think about placing one foot in front of another. Over time this action became automatic, and the need to think about it lessened. You stopped thinking about walking because the neuropathways in your brain have created a strong connection. A stroke damages neurons and breaks connections. The result is a loss of use of the affected body parts. The assumption once was that this lost connection was permanent. However, we now know that is false. Rewiring connections are possible with specific training. Neuroscience has shown that the brain constantly makes new connections even as we age.
Regaining some or all of your prior abilities will take time and work. Physiotherapists work to establish these new neuropathways.
Training must focus on creating mind and body connections. Repeatedly moving your hand will not make new connections. However, by moving your hand repeatedly while concentrating solely on the activity, you will begin to create new pathways by forcing your brain to send messages to fire neurons rapidly. Concentration is vital as research has shown that passive movements do not fire the brain neurons as much as active, concentrated activities.
Brain plasticity is a remarkable phenomenon. However, there are some points that you should realize. Treatment must be ongoing, repetitive, determined, and progressive. Age matters, and the brain of someone younger can regenerate nerve cells quicker than an older person. The brain can rewire itself for several years after a stroke. You should know that the rehab work will be challenging, and it will require steadfast dedication to push through in the weeks and months ahead.
Goal Setting
Setting goals is a crucial component in creating a successful stroke recovery plan. Working with your medical team to set realistic and measurable goals would be best. The entire stroke team should share your goals, and collectively everyone must work towards these goals.
It would be best if you took control of your stroke recovery. It is equally important that you establish a clear direction and have something tangible in front of you.
Consider breaking your big goals into small ones. Instead of saying I want to walk in three months, a reasonable goal might be that I intend to walk 10 meters in the next eight weeks. In the next four weeks, I want to be able to walk a few steps. In the next two weeks, I want to be able to move my thigh upwards while sitting. These are goals that follow the SMART system of goal setting.
SMART is an acronym for a proven successful method of setting goals.
S – Specific means you have identified the precise action you would like to do. Identify a specific activity or movement that you would like to achieve.
M – Measurable refers to a tangible way to measure your improvement. The goal should have a numerical component, such as walking 10 meters.
A – Achievable speaks to the fact that you must have high ideals, but they must be realistic. Push yourself with your goals, but you could set yourself up for failure if you reach too far.
R – Relevant goals are essential in the broader spectrum of the entire rehabilitation journey. Make sure your goals are specific to your recovery. Keep goals relevant to your recovery.
T – Time is the last component of goal setting. It is crucial to attach a time element to each goal. It is meaningless to say, ‘My goal is to walk around the block in my neighbourhood.’ A time-sensitive plan would change that to ‘I want to walk around my neighbourhood within six months.’
It is imperative that setting your goals collaborates with your stroke team. Everyone should be aware of what they want to achieve, and everyone should work towards that goal.
Benefits of Home Physiotherapy
If you are a stroke survivor and have spent some time in a hospital setting, you know how vital a physiotherapist is in your recovery process. Once discharged from the hospital, stroke survivors need to maintain their rehabilitation at home. It is essential to continue the recovery process, and you may have several options. You are returning to the hospital as an outpatient, attending a rehab or stroke clinic, or having a physiotherapist come to your home.
Continuing the recovery process at home presents many people with complex challenges. Home-based physiotherapy is challenging to obtain, very beurocratic, and not always ideally suited to the survivor’s specific needs. However, if you can receive high-quality care where the physio works one-on-one with you, that is the ideal way to accelerate your recovery.
There are many benefits of home physiotherapy. The most obvious benefit is that it gives peace of mind to stroke survivors that they do not have to worry about getting to a rehab facility. In Canada, winter poses significant transportation challenges. If you have reduced mobility, getting to and from a clinic is difficult.
A neuro-trained physiotherapist does not need gym equipment. Their primary tools are their hands and your home setup (steps, counters, chairs, recliners, etc.).
They use manual therapy and the patient’s body to continually rewire and reactivate your neuro pathways.
Another benefit of having a physiotherapist visit you is assessing you in your home environment. They will observe potential obstacles and alert you to potential dangers. It will also help them understand your home’s unique nature and how you navigate within it.
You will do the exercise using the available items in your home. These same exercises will allow you to continue in between your physiotherapy sessions. Remember repetition of movements in a mindful manner is the key to creating new pathways. Your physiotherapist will teach you how to use proper movement patterns for many of your daily activities. Compensation through wrong movement patterns is one of the main reasons you might not improve.
Home physiotherapy is usually a dedicated one-hour session of one on one therapy. In a rehab facility, therapists often deal with more than one client at a time.
In-home physiotherapy offers much more than convenience. It elevates your rehabilitation with a dedicated one on one therapy session.
Here at Bergin Motion, we have provided home physiotherapy in Barrie, Ontario and the surrounding areas for many years. We know the value that we provide to our clients on their road to recovery.
Resuming Activities
There are no specific guidelines for when to resume activities after a stroke. Every stroke survivor’s recovery is unique to them and their situation. It is crucial to begin moderate activities as soon as you are able. Exercise is key to helping people recover from a stroke.
Safety should be the primary focus during exercise after a stroke. If you have weakness in your arms or legs, then swimming and bike riding will pose safety concerns, and your therapist might recommend walking with a walking aid such as a cane or rollator.
Exercise is critical in helping to lower your blood pressure. Stroke survivors have an elevated risk of suffering another stroke, and the leading risk factor is high blood pressure.
In addition to helping to lower your blood pressure, exercise can help to reduce your cholesterol levels and lower your weight. Exercise has also proven to help reduce depression prevalent in stroke survivors.
Less than half of all stroke survivors do not get enough exercise after a stroke. Your overall recovery depends on activities done in a safe and secure environment. Make exercise part of your rehab program, and you will reap the rewards.
Avoiding Future Strokes
A very sobering statistic is that one in four stroke survivors will suffer another stroke in their lifetime. If you have suffered a stroke, you know the devastating effects that strokes can cause. It should motivate you to make the necessary lifestyle changes to decrease the chance of another stroke.
If you had a stroke and smoke, you are at higher risk of another stroke. The risk of smoking doubles your chances of a stroke. Quitting smoking is one of the hardest things one can do in their lifetime. However, if you match it up against the damaging effects of a stroke and the grueling rehab to recover, quitting smoking does not seem that difficult. It would help if you elicited as much help and support in your efforts to quit smoking. You owe it to both your friends, family, and most importantly, yourself to give every effort to make it happen.
If your doctor has prescribed medication to reduce your risks, you need to manage these medications effectively. Managing your medications can be very confusing. Seek help and stick to your schedule. Make sure that your doctor has a clear understanding of all your medications and ensure that different medications work well together.
Changes to your diet can reduce weight and balance your blood pressure and cholesterol levels. These are all important in reducing the chance for another stroke. The Mediterranean diet has proven to reduce the risk of strokes.
Unfortunately, stroke survivors run the genuine risk of suffering another stroke. However, they know the damage a stroke can inflict, hopefully motivating them to change their lifestyle choices. It is never too late to explore a NEW YOU.
Depression After a Stroke
It’s important to understand that there are additional risks after a stroke. Since strokes are a form of brain damage, there is a chance you might experience changes in mood and cognition. There is a risk of experiencing depression.
It is very typical to feel down after a stroke. Rehab is difficult and monotonous, and you can no longer do the things you used to do. However, consistently feeling down over some weeks might be a sign of depression. Depression is a genuine risk after a stroke. Make sure that you and your loved ones are aware of the dangers of developing depression. If a depressive mood continues, you should alert your doctor. Depression is treatable, and it is a recognizable medical condition. The stigma of depression is no longer what it once was, and if depression happens to you, consult your doctor and treat the ailment.
Your mood and personality may have slightly altered depending on the stroke location. Your family, friends, and support workers must know that you might have changed due to your stroke. Keep in mind that the brain is quite malleable and open to change. Hard work can help to repair the damage done to the brain.
Dementia After a Stroke
Evidence shows that the opportunities to develop vascular dementia increase after a stroke. Over one-quarter of all stroke survivors will develop vascular dementia within three months of a stroke. A network of arteries supplies blood to the brain. Disruption of blood supply to the brain is called vascular dementia. In the weeks and months following a stroke, you and your support team should stay alert to changes in memory recall, confusion, or inability to follow conversations. Early intervention can help to delay the effects of dementia.
The Sheer Power of Positive Thinking
The road to recovery may seem daunting. However, maintaining a determined and positive attitude is the most critical thing you can do to maximize your recovery. You are single handily the most important member of your rehab team. Your attitude and perseverance will be the significant determining factor in the level of success that your rehabilitation experiences.
Immerse yourself in your rehab as if your life depends on it. Challenge yourself day in and day out to keep focused, motivated, and active. Make sure you are challenging your mind as well as your body. Read more books and watch less tv as this will challenge your mind.
Enlist family and friends to push you when you inevitably hit the wall. Write motivational notes and place them throughout your home. Watch inspirational shows that can inspire you to keep moving forward.
Many stroke survivors have difficulty with the boredom and monotony of the rehab process and the painfully slow results. However, the successful stroke survivors push past this mental block and keep working towards their goal of regaining as much of their previous abilities as possible.
Stay focused, stay motivated and push through the long monotonous sessions. The rewards of doing the work will be life-changing.
Wrapping It All Up
If you are reading this book, you or a loved one has suffered a stroke. Hopefully, this article has enlightened you about the prevalence, causes, and recovery of strokes and given you hope that you can get better.
We know that strokes are all too standard, and they can rob us of movement and thoughts and alter our personality. Stroke survivors must be aware that they are at an elevated risk of suffering another stroke and consider necessary lifestyle changes.
Stroke survivors need to properly prepare their homes keeping safety and ease of mobility the primary objectives. Purchasing essential mobility and safety aids can significantly reduce the danger and stress of everyday tasks.
Assembling your support team is crucial in maintaining safety, living independently, and improving your odds of recovery. Your team should include both medical professionals as well as people to support you domestically as well as emotionally. Feeling supported can make a huge difference in your rehabilitation’s success or failure.
Working with a physiotherapist with experience treating stroke survivors will be crucial in your recovery process. If possible, find a physiotherapist who can come to your home and work with you in your environment.
Understand that you have suffered a brain injury. Your muscles can still function, but the signal to make them function has been interrupted. Through work with your physiotherapist, you can work to change your brain.
It will help if you believe in yourself and your desire to regain lost abilities. You are an essential part of your support team. It’s vital to understand that there will be tough times ahead. Your rehab will be monotonous, and at times the improvement will seem almost non-existent. However, you must never give up. Your brain can change, and you can make it happen.
Additional Resources
Stroke Recovery Time (Johns Hopkins Medicine)
About the Author
Sybille Bergin PT is a certified physiotherapist and one of the owners of Bergin Motion. Bergin Motion is a family-run Barrie Physiotherapy Clinic located in Barrie’s Southend. Sybille has been providing in-home physiotherapy for over 30 years. She specializes in treating acquired brain injuries, stroke recovery, and other related ailments.
Sybille is a certified NDT practitioner. Neuro Development Therapy is a specialized hands-on treatment technique that promotes mobility, balance, core strength, and gross motor skills in a playful, fun, and dynamic way.
Sybille leads a team of dedicated professionals providing first-class therapy at Bergin Motion to Barrie Ontario and surrounding areas.
Bergin Motion
Is a family owned physiotherapy company built by the Bergin family. Our family has served as physiotherapists in the Barrie area for over 30 years, spanning two generations. We are passionate about this community and helping people achieve their highest potential. Book with us now!